By Derek Hawn, Critical Care Paramedic – Tennessee
If you follow me on facebook, you’ve probably seen my posts and my work on first responder mental health. This is part of that same fight. Here in Tennessee, local news is running stories about people using rideshares instead of ambulances, and the drivers are saying they’re scared by what they’re being asked to do. At the same time, some people are pushing for nurse practitioners and physician assistants on ambulances like some kind of upgrade package. It’s time to say this clearly: EMS is healthcare, and the way this system treats both patients and providers is making us sick.
EMS is at a breaking point. Not because the medicine is too hard or because “nobody wants to work,” but because too many people with power still don’t understand, or don’t care, what EMS really is, what it costs, or who’s doing the work. As long as “ambulance driver” is the title, EMS stays undervalued, underfunded, and staffed by people who are burning out, developing PTSD and depression, and disappearing from rosters.
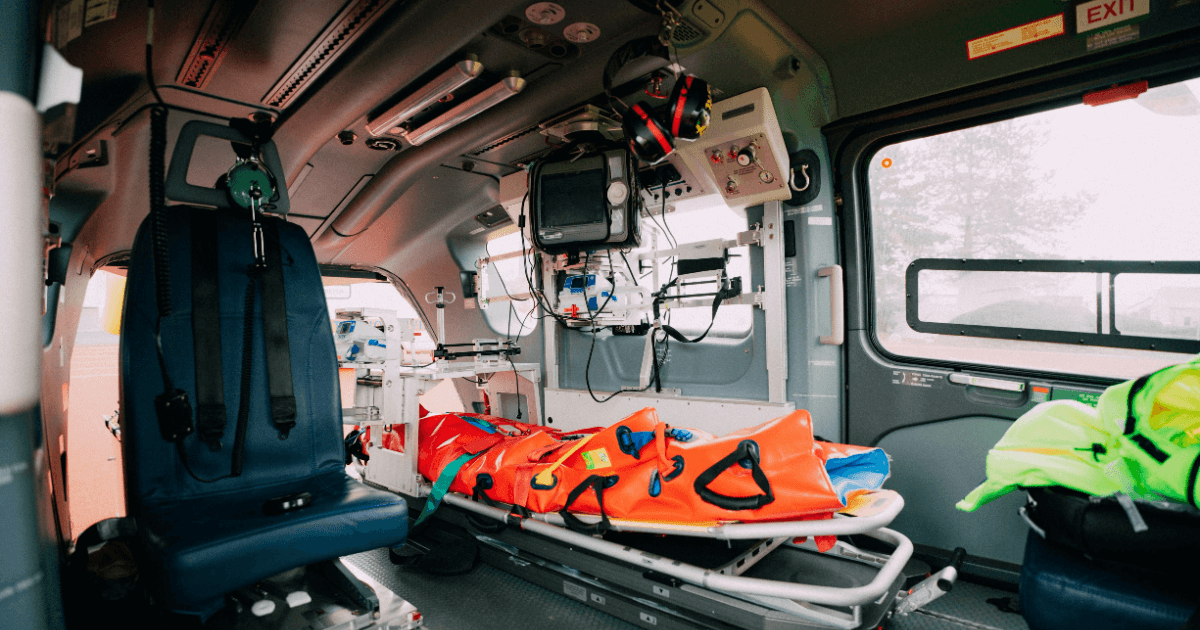
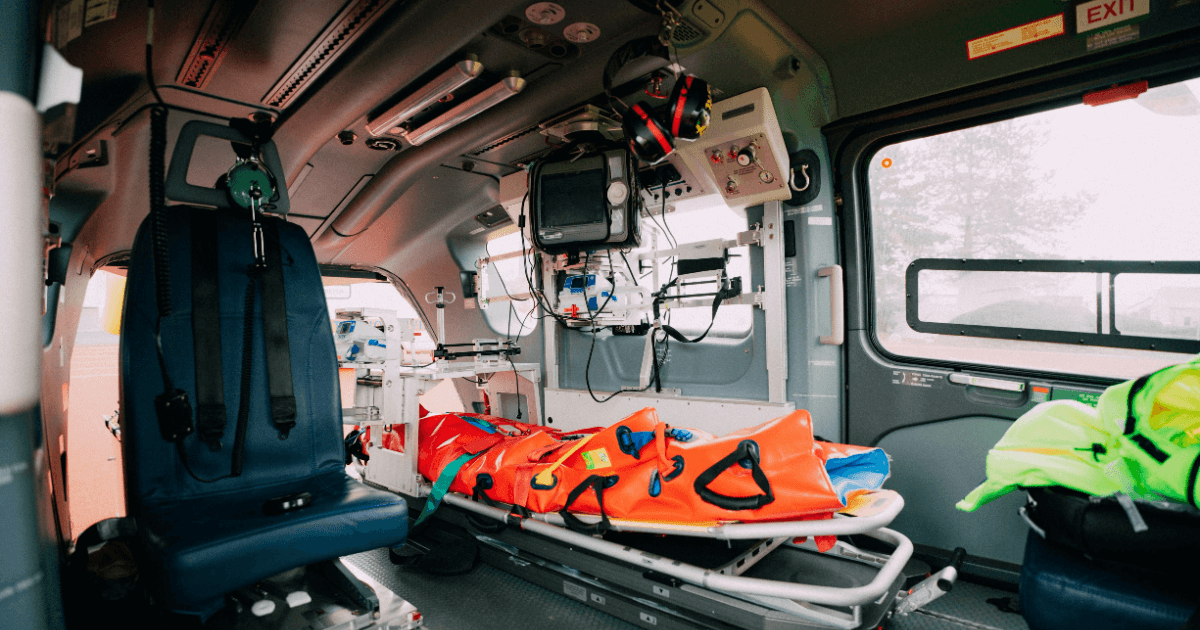
The rideshare instead of ambulance trend is not harmless. When news stories show drivers describing passengers with chest pain, severe shortness of breath, and other red flag symptoms, and saying they’re scared at being used in place of EMS, that’s a system failure, not a workaround. A rideshare sells you a seat and a driver. EMS brings you a mobile piece of the healthcare system, staffed and ready around the clock. You’re not paying for twenty minutes on a cot. You are paying for constant readiness: medications, monitor, ventilator, truck, fuel, maintenance, protocols, licensing, compliance, and the training that lets us walk in and take charge when everyone else is scared or frozen.
Most people never see that side. They see lights, a short ride, and a bill in the mailbox weeks later, with no explanation of why it costs what it costs. Instead of fixing funding and transparency, we’ve let the conversation turn into “ambulances are a scam” and “just call a uber.” People’s anger lands on crews who have absolutely no control over billing and spends their nights doing CPR on living room floors. It’s not just unfair. It’s one more weight on people who are already carrying everybody else’s worst days inside their heads.
Recently, a widely shared article in JEMS argued that the answer might be putting NP’s and PA’s on ambulances. The logic sounds familiar: medicine is more complex, liability is higher, expectations are bigger, so paramedics alone are no longer enough. What that framing leaves out is that EMS already has advanced clinicians, including paramedics, critical care paramedics, and community paramedics, who are specifically trained for prehospital decision making, and that adding mid level providers on top of a broken funding and staffing model doesn’t fix the problem that’s driving people out of this field.
Our classroom and clinical time are not built around quiet offices and scheduled follow ups. They’re built around high stake decisions in bad conditions with limited information and limited tools. We work in ditches at three in the morning, in single wides where you can barely turn around, and on rural highways where the nearest cath lab is an hour away. We do it while juggling endless call volume, hospital off load delays, and skeleton crews, all of which have been tied to higher burnout and mental health strain. We don’t need someone standing next to us to make us “real.” We need the system to stop pretending we’re not.
If you want the public to see EMS as healthcare instead of a taxi, start by showing them who’s actually on that truck.
When these roles are used fully, community paramedicine and integrated EMS programs reduce unnecessary 911 calls, avoidable emergency department visits, and preventable readmissions, while improving outcomes for high risk patients. For clinicians, that means fewer avoidable train wrecks and more chances to prevent the next crisis, which is a form of mental health protection in itself.
Put all of it together and EMS looks nothing like it’s made out to be in the comment sections. It’s response when someone’s having the worst day of their life. It’s critical care bridging hospitals for patients barely hanging on by a thread. It’s community paramedics keeping fragile neighbors from ever reaching that breaking point. It’s a real clinical continuum. The reason most people don’t know it is simple; for years, we’ve let other people define us, and some of them benefit from us staying small.
This is where culture and leadership come in, and where the mental health damage stops being theoretical. A lot of what’s breaking EMS isn’t happening in the back of the truck. It’s happening in offices. There’s still far too many “old school” chiefs and directors whose main goal is keeping public relations polished, not keeping providers alive and healthy. They love EMS Week photo ops. They don’t like the hard questions about pay, staffing, PTSD, depression, or suicide in their ranks.
You see that mindset every time someone comes back hollow eyed from a pediatric code or a gruesome fatality and hears, “suck it up.” Every time there’s no real critical incident policy, no structured debrief, no expectation that taking care of the provider is part of taking care of the community, leadership is making a choice, not a mistake. It’s a choice that raises the odds of that provider developing PTSD, depression, substance use problems, or just walking away from a profession they once loved. We talk a lot about resilience in EMS, but resilience is not forcing people to white knuckle their trauma in silence. Resilience is building systems where asking for help is normal and supported instead of punished.
State level EMS administrators don’t get a free pass either. When rules and protocols are written mostly by people who haven’t worked a modern ALS truck in years, if ever, you get fancy binders and miserable twenty four hour shifts. You get lowest common denominator protocols built around liability first and reality last. You get more training and documentation requirements with no talk about staffing or pay. You get appreciation weeks and hashtags while those same systems sign off on decisions that pile more weight on a shrinking pool of providers.
That’s not leadership. That’s self protection. It keeps the public in the dark about what’s really happening on the street. It slows or blocks the changes that would help the most, including expanding community paramedicine, better critical care capacity, real mental health programs, and real public education. And it sends one loud, clear message to EMS personnel:
Your trauma is your problem.
Your voice is a problem.
Your job is to shut up and drive.
If you expose people to death, suffering, and moral injury shift after shift, give them almost no say in how the system runs, and then offer almost nothing when the weight catches up, you don’t get “tougher” medics. You get people who leave, or stay and carry damage they never should’ve had to carry alone. The staffing crisis everyone suddenly wants to talk about didn’t appear out of nowhere. It was built, slowly and predictably, by choosing “no noise” instead of “do the right thing.”
So what do we do about it?
First, we stop being quiet about what EMS really is. We go into schools, churches, civic groups, council meetings, and explain in plain language what EMTs, AEMTs, paramedics, critical care paramedics, and community paramedics actually do. We bring the monitor, the medications, the airway kit, the ventilator, and the pump, and we connect them to real calls where those tools changed outcomes. We walk through chest pain, stroke, overdose, and trauma and spell out exactly why calling 911 is not the same as calling a rideshare, and what’s at stake when you get that choice wrong.
Second, we normalize talking about community paramedicine and critical care transport as standard parts of EMS, not pet projects. When taxpayers understand that EMS is keeping people out of the emergency department, reducing readmissions, and safely moving intensive care patients between facilities, it gets a lot harder to dismiss us as “ambulance drivers” and a lot easier to have conversations about funding and why an ambulance costs what it does.
Third, we start fixing our own house from wherever we stand. That means pushing for written critical incident policies that actually get used. It means building and defending peer support and counseling options that medics can access without being branded weak or unstable. It means real career ladders that recognize and reward advanced clinical roles like critical care and community paramedics as core pieces of the system, not side gigs for whoever is not already exhausted. It means creating real spaces where we can talk about what this job is doing to us, and make it ok to admit “we are not ok”.
Finally, we stop pretending that bad leadership is just “the way it’s.” When local or state level administrators cling to the “ambulance driver” era, block progress, and ignore the mental health and safety of their people, we call it what it is. We bring it up in staff and public meetings. We write about it. We organize around it. And when we get the chance, we vote and advocate for people who understand that EMS is healthcare and that the health of the system depends on the health of the people inside it.
EMS isn’t just lights and sirens. It’s resuscitation on a restaurant floor, intensive care rolling down the highway, and preventive medicine at a kitchen table. It’s EMTs, AEMTs, paramedics, critical care paramedics, and community paramedics holding communities together one call at a time. The public will not value what they don’t understand, and we will not get the support and mental health care we need as long as we let other people define us as “ambulance drivers.” It’s past time we tell our own story and insist that the people in charge, locally and at the state level, either stand up with us or step aside.

Put your business in front of thousands of LOCALS! Create your free listing on the NewsSTAND and update your profile anytime to share the latest info, specials, and contact details.
Got a story to Share? Pitch your idea or write an article for the NewsSTAND! Join us in highlighting the positive and powerful moments that make our city shine.

We’re passionate about working together to amplify our City. Reach out to the NewsSTAND team to explore collaboration opportunities and make a difference in our community.
Hover over each card to unlock the full story and see what you’re about to get!